Table of Contents
Differences between IBS and IBD
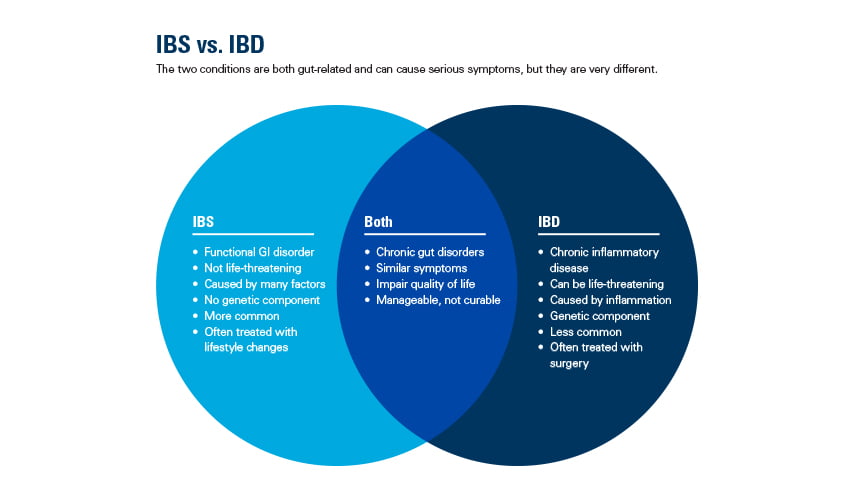
Irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD) are two common functional and organic gastrointestinal disorders that can cause similar symptoms like abdominal pain and changes in bowel movements. While they may seem identical on the surface, IBS and IBD have key differences in their underlying causes, mechanisms of action, and ultimate impact on the body [1].
IBS is classified as a functional bowel disorder that involves abnormal gut-brain signaling and intestinal motility without demonstrable inflammation or tissue damage[2]. In contrast, IBD arises from a misdirected immunological response that leads to chronic inflammation of the digestive tract. Crohn’s disease and ulcerative colitis are the main forms of IBD[3].
The symptoms, location affected within the gastrointestinal tract, diagnostic criteria, and typical treatments also differ between IBS and IBD [4]. Understanding where these conditions diverge is important for determining the proper evaluation and management approach by a medical provider.
While the following IBS or IBD quiz aims to aid in distinguishing these entities based on common symptom patterns, it is not intended as a substitute for an actual medical diagnosis. Anyone experiencing persistent or worsening gut issues should consult their doctor to undergo a complete evaluation and receive a confirmed diagnosis. Let’s now review some key aspects of how IBS and IBD compare.
Do I have an IBS or IBD Quiz (5 questions)
The following questions can help you identify symptom patterns and guide a conversation with your doctor. However, these results are only a starting point and not a replacement for medical advice.
- How often are your symptoms present?
IBS causes intermittent flare-ups separated by symptom-free periods lasting days to weeks.[5] Flare-ups are often triggered by stress, diet, or missed meals. IBD results in continuous symptoms present most days of the week that are persistent and unpredictable[6].
- What is the nature of your bowel movements?
IBS can cause loose stools, diarrhea, or constipation. Stools remain non-bloody. IBD commonly produces bloody stools containing mucus or pus due to intestinal inflammation physically damaging the colon lining [7].
- Where do you feel abdominal pain or discomfort?
IBS pain is localized to the lower abdomen and usually worsens with bowel movement. IBD pain can originate in the lower gut but sometimes radiates to other areas of the GI tract like the back or anus due to transmural inflammation throughout the digestive wall[8].
- Have you experienced any systemic symptoms?
IBS triggers only cause gut symptoms like changes in bowel habits. IBD is associated with constitutional symptoms such as fatigue, weight loss, and fever resulting from chronic disease burden[9].
- Is there a family history of intestinal disorders?
IBS does not appear to have a hereditary basis. A family history of IBD such as Crohn’s disease or ulcerative colitis increases one’s own risk due to shared genetic factors[10].
When to See a Doctor
While the IBS or IBD quiz can offer clues about the likely cause of your digestive symptoms, it cannot provide a definitive medical diagnosis. An in-person evaluation is necessary to properly differentiate between these conditions and rule out other potential issues.
Seeking medical advice is particularly important if:
- Your symptoms are severe or interfering with daily life. Unrelenting abdominal pain or diarrhea need to be examined.
- You experience weight loss, blood in stool, or other alarming symptoms beyond just changes in bowel habits. These could indicate something more serious than IBS.
- Symptoms do not resolve after making recommended dietary or lifestyle changes. Lingering issues warrant professional guidance.
- You have a family history of IBD or other inflammatory gut diseases. Genetic risks need clinical screening.
- Your symptoms started abruptly, especially after age 50. This timing may point to other underlying problems.
By consulting a doctor, tests can be ordered to examine the gastrointestinal tract, checks for inflammation done, and other conditions excluded. A formal diagnosis allows targeted treatment best suited to each individual’s needs.
While the IBS or IBD Quiz aims to provide insight, it is not a substitute for an actual clinical evaluation. Anyone with ongoing or worsening digestive issues should see their healthcare provider for definitive next steps.
Additional Conditions to Consider
It’s important to note that this informal IBS or IBD Quiz only screened for common symptoms. While the two are among the most common functional and inflammatory bowel diseases, they are not the only potential causes of gastrointestinal symptoms. Other medical issues that can mimic or overlap with IBS/IBD include:
- Celiac Disease: An immune reaction to gluten that damages the small intestine. Screening includes blood tests and biopsy.
- Colorectal Cancer: Unexplained change in bowel habits, blood in stool, and weight loss beyond IBS scope warrants cancer exclusion by colonoscopy.
- Lactose Intolerance: Inability to digest dairy due to lactase deficiency, triggering diarrhea. Confirm via elimination diet or breath test.
- Small Intestine Bacterial Overgrowth: Excess bacteria in the small bowel cause bloating, gas, and altered stools. Testing includes lactulose breath test.
- Gastroenteritis: Exposure to infections like C.difficile or norovirus can acutely disrupt digestion in a similar way to IBS.
- Diverticulitis: Swelling or infection of pouches protruding from the colon necessitating imaging scans.
- Colon Polyps: Non-cancerous growths which, if left, could transform into colon cancer over time. Visualized during colonoscopy.
Seeking medical evaluation helps rule out additional organic illnesses playing a role in worsening GI distress beyond what IBS alone could cause. An exclusion process confirms the correct diagnosis.
Conclusion
In summary, distinguishing between IBS and IBD based on symptoms can provide insights but is not a substitute for a full medical workup. The IBS or IBD quiz serves as a starting point to help identify whether the pattern of digestive issues experienced aligns more closely with IBS or the potentially more serious IBD.
Obtaining an official diagnosis through consultation with a doctor is necessary to confirm the specific condition, exclude other potential organic causes that may require different management approaches, and determine appropriate long-term treatment. Symptom relief and disease control are best achieved under professional medical guidance tailored to individual needs and presentation.
While IBS and IBD share some overlapping gastrointestinal complaints, understanding how their underlying disease mechanisms, common symptoms, diagnostic criteria, and treatments compare can aid decision-making around when to seek evaluation. Consulting a gastroenterologist promptly about persistent or worsening abdominal distress helps optimize health outcomes.
With clinical support and proper management, it is possible to effectively live with either IBS or IBD. Continued education on distinguishing key aspects between the two empowers people to help pinpoint concerns and access the care that is right for their unique situation.