Table of Contents
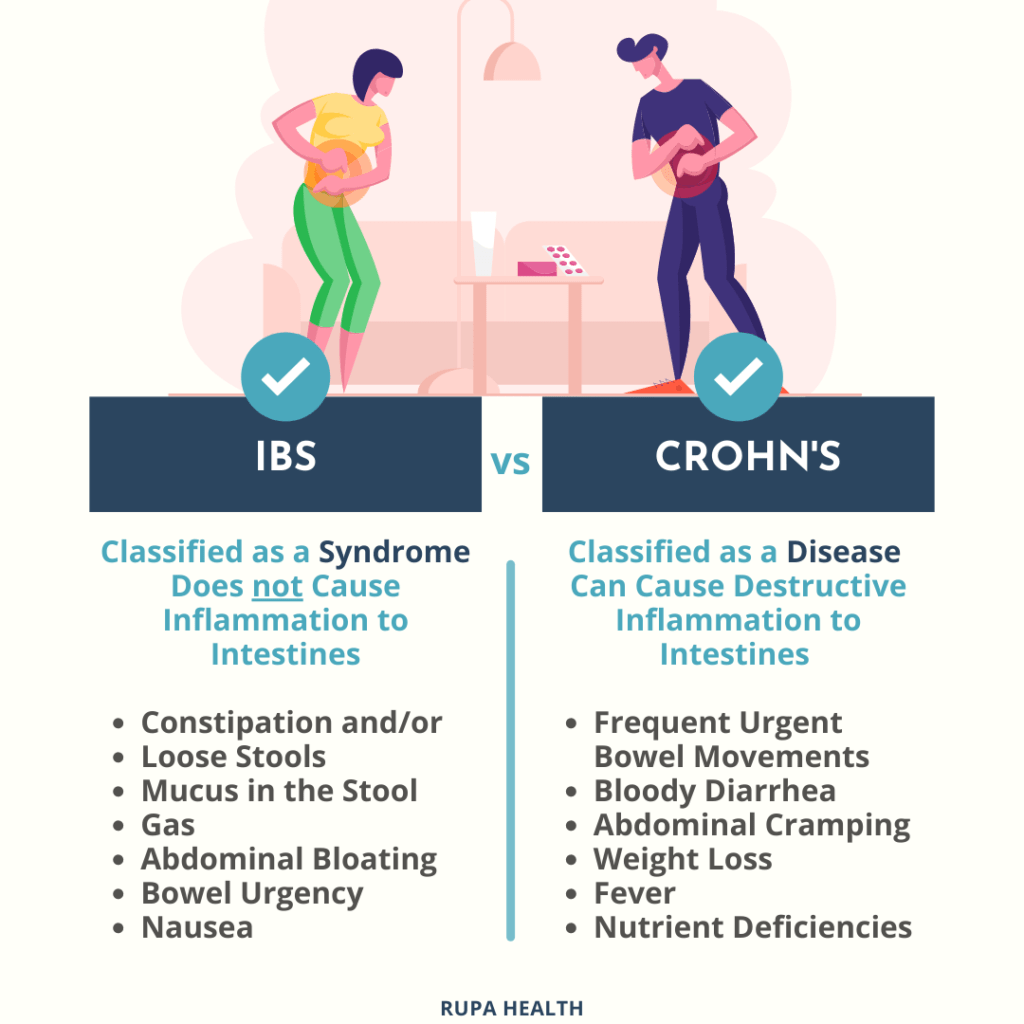
Differences between Crohn’s Disease and IBS
This “Do I Have Crohn’s Disease or IBS Quiz” will help identify if you have Crohn’s disease or irritable bowel syndrome (IBS) as such Gastrointestinal diseases can be difficult to differentiate based on symptoms alone. According to a 2017 study in Clinical Gastroenterology, up to 25% of patients given a diagnosis of IBS may in fact have inflammatory bowel disease (IBD) like Crohn’s disease[1]. While IBS is considered a functional gastrointestinal disorder, Crohn’s disease is an inflammatory condition that requires appropriate treatment.
Crohn’s disease and IBS share some common symptoms such as abdominal pain, diarrhea, and changes in bowel habits. However, Crohn’s disease differs in that it is a chronic condition involving inflammation of the digestive tract [2]. Symptoms tend to come and go with IBS, while Crohn’s disease symptoms persist and may worsen over time if left untreated. Additional indicators of Crohn’s disease include weight loss, bleeding, and frequent bouts of severe diarrhea [3].
This “Do I Have Crohn’s Disease or IBS Quiz” is not intended as a substitute for a medical diagnosis. The responses simply provide a general idea of which condition your symptoms appear to align with more closely based on typical presentations. However, symptoms can vary significantly in both Crohn’s disease and IBS. The only way to obtain an accurate, confirmed diagnosis is through thorough physical examination and potentially diagnostic tests ordered by your doctor.
Do I Have Crohn’s Disease or IBS Quiz (8 Questions)
The following questions can help you identify symptom patterns and guide a conversation with your doctor. However, these results are only a starting point and not a replacement for medical advice.
- Have you experienced ongoing abdominal pain and discomfort at least once a week over the past three months?
Abdominal pain is a common symptom of both Crohn’s disease and IBS. For people with Crohn’s, the pain is often located in the lower right area of the abdomen where the ileum and colon are found. However, the location alone does not differentiate the conditions. What’s more important is how frequent, severe, or limiting the pain is. Ongoing pain occurring at least weekly could point to Crohn’s.
- Do you alternate between constipation and diarrhea?
Many people with IBS experience switching back and forth between constipation and diarrhea, known as IBS with mixed bowel habits (IBS-M). Crohn’s more typically involves diarrhea but usually not constipation. It’s important to pay attention to stool consistency patterns over time and how they impact daily life.
- Do your symptoms improve after having a bowel movement?
For those with IBS, abdominal discomfort and changes in bowel habits tend to relate directly to the act of having a bowel movement. Symptoms often subside completely afterwards. With Crohn’s, symptoms may not always correlate as strongly with bowel movements due to deeper intestinal inflammation.
- Do you experience anxiety or depression?
Research has shown that psychological factors like stress, anxiety and depression can exacerbate IBS symptoms for some individuals by impacting the gut-brain connection [4]. A history of mental health concerns points to the potential role of the mind-gut axis in gastrointestinal issues.
- Are you prone to developing mouth sores or ulcers?
Oral ulcers and sores are common in around 20-50% of Crohn’s patients, especially during flare-ups, as the disease can involve any part of the digestive tract [5]. Mouth problems point more specifically to Crohn’s versus IBS where gastrointestinal issues are usually confined below the stomach.
- Do you experience fatigue or weakness?
Irritable bowel symptoms do not typically cause systemic fatigue, while Crohn’s is considered a systemic disease associated with increased whole-body inflammation, nutritional deficiencies, anemia, and consequently fatigue that interferes with activities of daily living.
- Do you have unexpected weight loss?
Unintended weight loss may occur with Crohn’s due to reduced appetite and impaired absorption of nutrients from the small bowel inflammation. Weight normally remains stable with IBS unless other medical causes are involved.
- Do you experience rectal bleeding or blood in your stools?
Visible bleeding in the toilet or on toilet paper is abnormally concerning and requires prompt medical evaluation to identify potential causes like inflamed bowel tissue in Crohn’s disease versus hemorrhoids. Bright red blood especially needs attention.
When to See a Doctor
While taking the “Do I Have Crohn’s Disease or IBS Quiz” can provide insight into your symptoms, it is not a substitute for an in-person medical evaluation. Seek prompt medical attention if you experience:
- Persistent or severe abdominal pain that wakes you at night or interferes with daily life
- Changes in bowel habits along with unintended significant weight loss
- Rectal bleeding on a regular basis
- Fever accompanied by abdominal issues
- Diarrhea that will not improve within a few weeks
- Abdominal pain or tenderness upon examination
Additionally, speak with your doctor if:
- Symptoms are ongoing and recurrent over several months
- Symptoms severely impact your quality of life
- You have a family history of Crohn’s disease or other IBDs
- New symptoms develop such as joint pain or lesions on the skin
Seeing a healthcare provider is important to rule out potential complications, get appropriate tests, and start treatment if a chronic condition is detected. Don’t ignore persistent symptoms – address any concerns with your doctor sooner rather than later.
Additional Conditions to Consider
It’s important to note that this informal “Do I Have Crohn’s Disease or IBS Quiz” only screened for symptoms commonly seen in Crohn’s disease and IBS. There are several other gastrointestinal (GI) conditions that could cause similar symptoms, including:
- Celiac disease – An immune reaction to eating gluten that damages the small intestine.
- Ulcerative colitis – A form of inflammatory bowel disease (IBD) that causes ulcers and inflammation in the colon.
- Gastroesophageal reflux disease (GERD) – Chronic reflux of stomach acid that can trigger a wide range of GI issues.
- Lactose intolerance – Difficulty digesting the sugar in dairy due to lactase deficiency.
- Infectious colitis – Colon inflammation caused by bacteria, viruses or parasites.
Given the range of potential GI diagnoses, discussing your full medical history and family history with a gastroenterologist is recommended. This will help rule out other underlying conditions.
Conclusion
In closing, remember that this “Do I Have Crohn’s Disease or IBS Quiz” merely serves as a starting point to identify which common gastrointestinal condition your symptoms seem to align with most. The goal is to help you start an informed discussion with your doctor about any issues you may be experiencing. However, an actual confirmed diagnosis can only be provided through comprehensive medical tests and evaluation as individual presentations may vary or overlap between conditions. Your health and honest reporting of symptoms is important to receive the care needed. We thank you for your time and wish you the very best in feeling your best.