Table of Contents
Introduction
Irritable bowel syndrome (IBS) is one of the most common gastrointestinal disorders, affecting up to 1 in 5 people worldwide. Common symptoms include abdominal pain or discomfort, bloating, gas, diarrhea, and/or constipation[1]. While typically confined to the abdominal region, many IBS sufferers report nonspecific pain in other parts of the body as well and this post explores if can IBS cause testicle pain.
Some anecdotal evidence and case studies point to a potential link between IBS and testicular discomfort[2]. However, a direct link has yet to be conclusively proven. This post explores the hypothesis that IBS may in some instances contribute to or cause pain in the testicles through various proposed mechanisms of action.
Can IBS cause testicle pain? (Other Causes)
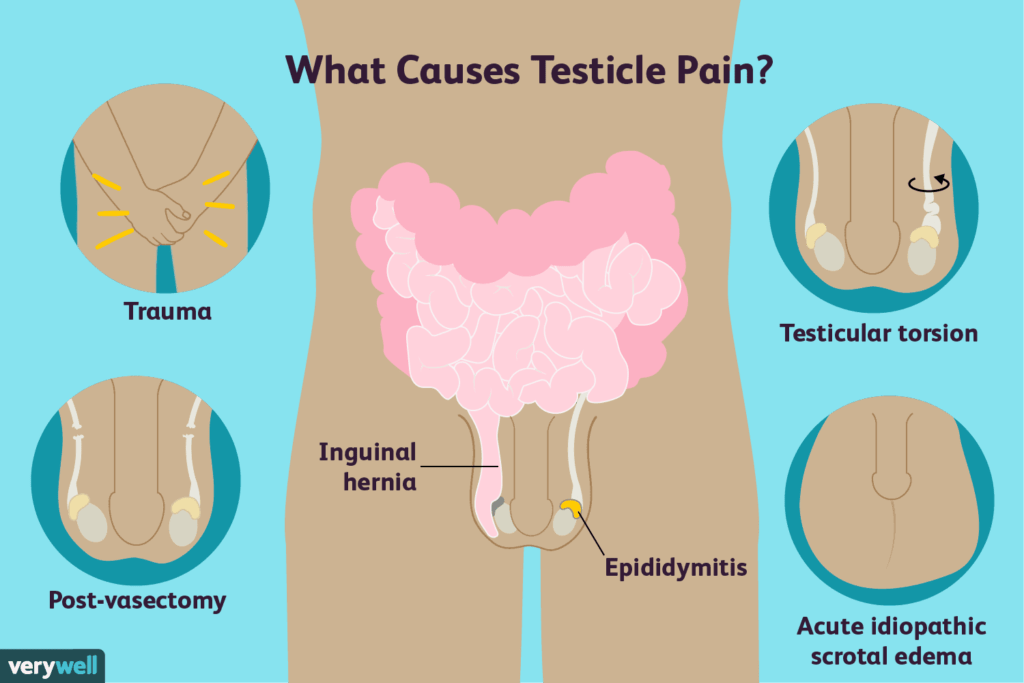
Testicular pain or discomfort can arise from several conditions affecting the testicles or surrounding structures. One potential cause is infection, such as epididymitis which involves swelling or inflammation of the epididymis tube that transports sperm. Direct blunt force trauma from an injury is another common reason for testicular pain, as the tissue is vulnerable to impact[3].
Testicular torsion involves twisting of the spermatic cord, cutting off blood supply, and potentially causing necrosis if not quickly treated. A varicocele refers to enlarged veins within the scrotal sac, common in up to 15-20% of adult men, which can sometimes lead to dull pain[4]. Distinguishing these potential anatomical or infectious causes from non-organic sources of pain is important in asking “Can IBS cause testicle pain” prior to considering potential links to functional disorders.
Pathophysiology of IBS
While the underlying causes are still under investigation in asking “Can IBS cause testicle pain”, abnormal gastrointestinal function appears central to IBS. Heightened sensitivity of the gut-brain axis and visceral hypersensitivity occur in IBS patients, meaning they perceive non-painful stimuli as painful. Motility issues in alternating directions like constipation or diarrhea are also factors[5].
The mechanisms driving such gut hypersensitivity are complex but likely involve genetic and environmental triggers that alter pain-signaling pathways in the gut and brain[6]. A greater understanding of the pathophysiology helps build potential links between IBS and referred pain in other regions.
Potential Mechanisms
To answer “Can IBS cause testicle pain”, Referred pain is one proposed explanation for testicular discomfort in IBS patients. It occurs when a visceral pain stimulus activates shared neurological pathways, leading to the perception of pain in another region of the body innervated by related nerves[7].
There is an overlap between the nerves supplying the gastrointestinal tract and the genitourinary system which could allow for bidirectional referred sensations. The hypogastric nerve plexus transmits sensory information from the pelvis and lower abdomen up to the spinal cord. Simultaneously, splanchnic nerves conduct signals descending from the brain[8].
Heightened sensitivity throughout the gut-brain axis in IBS may lower pain thresholds in other body parts with interconnected innervation. Previous research has demonstrated increased reactive responses even to non-painful rectal distension in IBS, indicating widespread visceral hyperalgesia[9].
Differential Diagnosis
To answer “Can IBS cause testicle pain” it’s important to evaluate testicular pain, to first distinguish potential organic causes from functional etiologies like referred pain from IBS. Other infectious etiologies should be ruled out through physical examination and testing, as they may require specific antimicrobial treatment. Acute epididymo-orchitis or epididymitis can cause inflamed, tender orchitic testes and will commonly be associated with urinary tract infection symptoms like dysuria[10].
Chronic or intermittent testicular pain may indicate a structural issue like varicocele that requires imaging evaluation. Scrotal ultrasound is the initial recommended imaging modality to identify lesions, cysts, tumors, or varicoceles that need urologic management[11]. For cases of recurrent or persistent undiagnosed pain, a referral to a urologist is important to examine for occult testicular torsion, hydrocele, or other intra-scrotal abnormalities. Performing a physical exam under anesthesia allows thorough palpation of all scrotal contents.
If standard imaging and exploratory surgery rule out anatomical issues, functional causes like referred pain should be explored. Given a concurrent diagnosis of IBS, a trial of conservative therapies targeting the underlying bowel dysfunction may help determine the likelihood of an association between the two conditions.
Management
Lifestyle modifications that can help alleviate IBS symptoms may also provide relief from associated testicular discomfort. A low FODMAP diet aims to reduce gut distension and fermentation by limiting certain poorly absorbed short-chain carbohydrates[12]. Stress management techniques like yoga and meditation can regulate the gut-brain axis involved in visceral hypersensitivity.
If dietary and lifestyle changes provide insufficient relief, medications may help reduce abdominal pain believed to be contributing to referred testicular pain. Antispasmodics like dicyclomine mitigate gut motility issues while tricyclic antidepressants can modulate visceral sensory pathways[13].
Pelvic floor physical therapy targets muscle tension and tenderness that may influence viscerosomatic referral patterns[14]. Myofascial release techniques and biofeedback train relaxation of overactive pelvic floor musculature[15].
Surgery should only be considered if pain persists after conservative options and if other anatomical pathologies have been thoroughly excluded by imaging and urological evaluation. Surgical intervention solely for assumed referred visceral causes would carry risks unsupported by conclusive evidence.